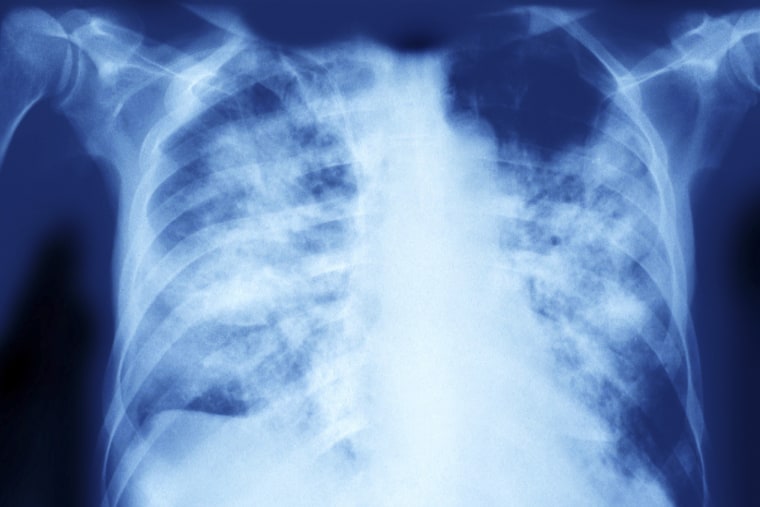
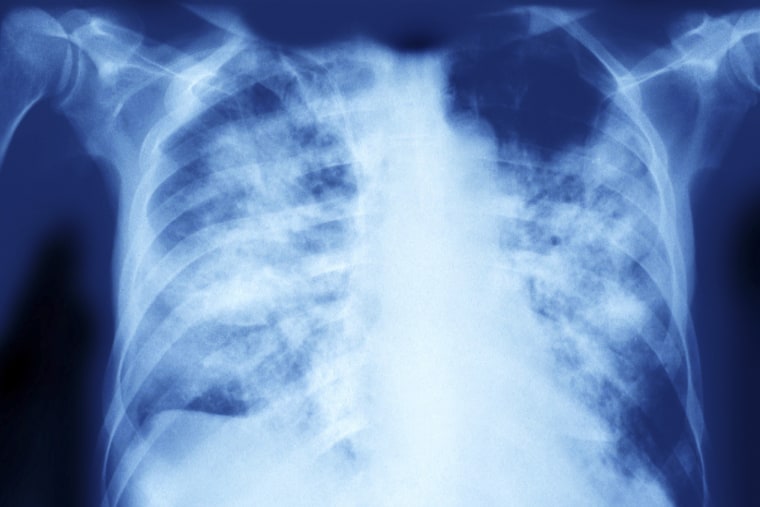
Franklin Dobbs, a 76-year-old affected person of Pappas’, additionally had pre-existing lung issues earlier than he was identified with aspergillosis final 12 months. Dobbs stated he hemorrhaged on and off for a few 12 months earlier than getting identified. His case has up to now not proved drug-resistant.
An azole referred to as Noxafil improved his signs, Dobbs stated, although he nonetheless feels weak.
“I’m still having a problem with the strength in my legs,” he stated.
Dobbs believes he may need been uncovered whereas planting tomatoes, corn and peas within the backyard, or whereas constructing birdhouses outside.
An April study discovered that individuals can get contaminated with drug-resistant Aspergillus from their house gardens. The researchers collected lung samples from contaminated sufferers within the U.Okay. and Ireland, and matched a few of them to drug-resistant strains within the environments close by.
Sometimes, a single high-dose publicity, resembling a cloud of spores launched by digging in soil, may be sufficient to set off a fungal an infection. But in lots of circumstances, folks are steadily uncovered to Aspergillus over months earlier than they turn out to be sick.
“This is an extremely concerning superbug-type situation,” Armstrong-James stated. “We’re all inhaling this all the time. So potentially, we could all be inhaling resistant Aspergillus on a daily basis.”
Unlike Aspergillus, Candida auris is generally detected in hospitals, amongst folks who are on respiration or feeding tubes or receiving a central line (an IV catheter that administers fluids, blood or medicine).
“When you have one of those medical interventions that are in patients, you become at risk of it getting into your bloodstream or creating an abscess, and that’s when it’s very dangerous,” stated Luis Ostrosky, chief of infectious illnesses at UTHealth Houston and Memorial Hermann Hospital.
More than 90% of Candida auris strains are proof against the frequent azole fluconazole, and as much as 73% are resistant to a different referred to as voriconazole. Some strains even have resistance to the drug Fairweather not too long ago stopped taking.
“You can end up with a patient with a Candida auris infection where you actually don’t have an antifungal to use for that patient. It’s resistant to everything,” Ostrosky stated. “Basically those patients go to hospice and die, and there’s nothing you can do.”
Why mould is rising proof against medicine
Researchers have pinpointed two essential drivers of antifungal resistance: human medicine and chemical substances utilized in agriculture.
Farmers typically rely on fungicides, however over time, sure strains of mould turn out to be resistant. And since fungicides are chemically just like antifungal medicine, some mould strains develop resistance to the medicines too.
The 65-year-old man who died of invasive aspergillosis, for example, was infected with a strain linked to agricultural fungicide use, in keeping with the CDC.
“Bulbs and onions that have been dipped in these antifungals so they don’t spoil are almost like time bombs. When they’re planted, the fungicides that are on their surface will leak out into the environment,” stated Armstrong-James, who co-authored the April examine on Aspergillus.
“That could be a key breeding ground for resistance,” he added.
Drug use contributes to resistance when antifungal medicine are prescribed too typically, or if medical doctors do not prescribe a excessive sufficient dosage or lengthy sufficient therapy course. That can then put selective strain on fungi.
“The more you use antifungals or antibacterials, the more resistance that you see,” Pappas stated.
Armstrong-James stated that hospitals see resistance to Candida auris extra continuously than to Aspergillus.
“Every time anyone takes fluconazole, you can get Candida resistance,” he stated.
Climate change and Covid might every play a task
Climate change could also be catalyzing the unfold of each Aspergillus and Candida auris.
That’s as a result of rising temperatures can result in extra fungicide resistance. Some analysis means that climate change was a key driver of Candida auris’ first appearance in people in 2009.
“Within a very short period of time, you’ve got the emergence of four or five different families of Candida auris more or less co-emerging simultaneously. How does that happen? It really screams if there’s something going on in the environment,” Pappas stated. “There’s decent evidence that climate change is at least one of the triggers.”
Some specialists fear that as local weather change’s results intensify, even some wholesome folks may get fungal infections.
“Whilst there’s no evidence for the moment that a perfectly well person could get a severe Aspergillus infection, there’s nothing to say that, with the changing environments, that might not change in the future,” Armstrong-James stated.
On high of all this got here the Covid pandemic, which created new alternatives for Candida auris to unfold. A July CDC report discovered that these infections rose 60% in well being care settings from 2019 to 2020.
“Invasive Candida infections just skyrocketed with Covid, presumably because all these patients were sick,” Pappas stated. “They were given broad spectrum antibiotics. They had lines and ventilators and all the things that you need to generate invasive Candida.”
The CDC report discovered that staffing shortages and prolonged affected person stays, amongst different components, made it tough for some hospitals to forestall drug-resistant infections.
“We were having all these traveling nurses that came from different parts of the country that weren’t necessarily attuned to the protocols that the hospital normally has to prevent bloodstream infections,” Ostrosky stated.


New therapy choices may take years
Doctors say they’re in a race in opposition to time, since present therapies may cease working earlier than new ones turn out to be accessible.
“If we don’t handle resistance proper now and if we don’t enhance the pipeline for the antifungals, we might very simply find yourself in a spot in 5 to 10 years the place you’re having end-of-life discussions with a affected person that has an invasive Candida an infection,” Ostrosky said. “It’s simply unthinkable proper now that the one you love can go into the hospital and have an appendectomy, they usually get a complication, they usually find yourself with a bug that’s untreatable.”
Several drugs have entered late-stage studies that could produce results in the next year or two, experts said.
But Fairweather isn’t sure she’ll get a chance to try them.
“How a lot harm shall be executed to my lungs earlier than this stuff come into impact?” she said.
Plus, fungi could develop resistance to new medications over time.
“Once they’re on the market, they get overused after which fairly rapidly, they’re now not helpful,” Pappas stated.


